Blood health and homeostasis are rarely talked about until there’s a big problem (read: you get a blood clot), so you probably haven’t heard much about hypercoagulation (think sticky, thick blood, with an increased clot risk).
Western medicine does not do a great job at preventing thrombotic events like blood clots and deep vein thrombosis (VTE). Reasons being — screening is expensive, genetic risk factors are not common enough for general public screening, and genetic testing for asymptomatic persons may induce undue stress.
Western medicine’s purpose is treating and managing disease, not preventing it.
But what if you were to instead view good blood circulation like that as a nutrient, and address it proactively?
IMPORTANCE OF GOOD CIRCULATION
If you were to take all the blood vessels out of an adult body (talking about arteries, veins, capillaries) and lay them out in a straight line, it would end up spanning a length of approximately 100,000 miles. [10]
This is the highway for your immune system as well as for your body to deliver oxygen, nutrients, and hormones to cells as well as remove waste products.
What if your circulation highway is more like a 5’clock traffic jam due to thick, sticky blood slowing down the flow of ‘traffic’ in your bloodstream?
How is that going to make you feel?
If you’re thinking perpetually inflamed, overly sensitive, chronically ill, and fatigued — you’re on to something…
When nutrients and toxins are slowed in transit, the outcome isn’t going to be great for how you feel.
Your cells get starved of nutrients and oxygen as well as toxins hang out in your body longer than they should…
WHEN COAGULATION AND CIRCULATION GOES WRONG
Blood clotting serves an important job in the body. When you cut your finger, it’s the coagulation cascade that initiates the clotting process to prevent excessive bleeding and blood loss. Inflammation, however, can cause your coagulation cascade to go rouge.
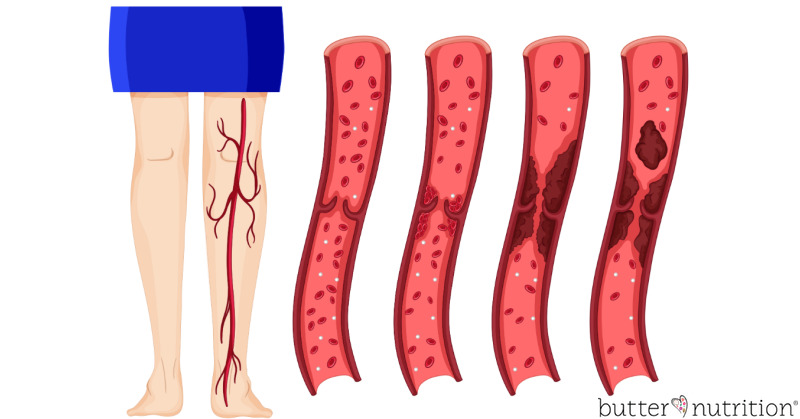
Chronic inflammation triggering hypercoagulation causes a fibrin layer (think tough protein mesh-like buildup) to get deposited along your blood vessel walls. This further impedes circulation by reducing blood flow. It’s as if your circulation superhighway not only is a traffic jam by sticky, thick blood, but now a lane is blocked or closed by way of fibrin buildup. The buildup of fibrin can also serve as a protective biofilm, creating a safe haven for infections, viruses and pathogens to hide from your immune system. [4]
SIGNS OF HYPERCOAGULATION
Normally when people think of hypercoagulation, it’s mostly in relation to cardiovascular disease — heart attack, stroke, and hypertension. But what about hypercoagulation’s links to inflammatory bowel disease, migraines, diabetes, varicose veins, hemorrhoids, and chronic fatigue? [9]
Perhaps hypercoagulation is a lot more common than previously thought.
Do any of these signs of hypercoagulation look familiar to you?
- pale, swollen tongue with scalloped edges
- brain fog, anxiety, irritability
- poor AM appetite
- exercise intolerance
- mottled skin
- cold/clammy hands and feet
- sensitive teeth
- limbs fall asleep easily
- insomnia, restless leg syndrome
- ‘doughy’ and tender abdomen
- red/purple feet, edema in legs
- mast cell activation syndrome (MCAS, associated with abnormal coagulation)
RISK FACTORS/CONDITIONS THAT LEAD TO MORE HYPERCOAGULATION
Hypercoagulation often has underlying causes or risk factors that upset the balance of the coagulation cascade, encouraging a tendency towards clotting over blood thinning mechanisms. Most simply, inflammation triggers a hypercoagulative state [11], but you also have to identify and address the root cause of of the inflammation.
- toxicity, causing a sluggish liver and biliary system
- genetic factors, 20% have a genetic predisposition (see testing details below)
- increasing age
- major surgery
- cancer
- mold
- chronic stress
- immobilization
- dehydration
- viral infections
- bacterial infections (especially gut infection due via endotoxin)
- inflammatory bowel disease (IBD)
- infections, especially chronic gut infections
- estrogens (especially birth control pills, etc.)
- underlying inflammation
- pregnancy
- obesity
- smoking
TESTING FOR HYPERCOAGULATION
From my exposure, testing for hypercoagulation is not common, especially in Western medicine. If you are interested in testing, you may need to find a hematologist, functional or naturopathic doctor to run coagulation labs for you. Here are some of the most common labs used to assess coagulation:
- Antithrombin III – a powerful anticoagulant
- Protein S — act as the ‘brakes’ on clots (deficiency, seen in liver disease, vitamin K deficiency, hereditary deficiency)
- Protein C — act as the ‘brakes’ on clots (deficiency, seen in liver disease, vitamin K deficiency, hereditary deficiency)
- Homocysteine
- D-Dimer
- Fibrinogen Activity
- Plasminogen Activator Inhibitor (PAI-1)
- Factor II Activity
- Prothrombin Fragment 1 + 2
- Anti-thrombin Activity
- Lipoprotein (a)
- Alpha-2-Antiplasmin
- Genetic testing — Factor V Leiden (F5, see below)
- Genetic testing — Prothrombin g20210a (F2, see below )
- Genetic testing — Antithrombin III deficiency (rare)
GENETIC FACTORS
There are two main genetic factors to look out for that will predispose one to hypercoagulation or a greater tendency towards blood clotting — Factor V Leiden and Prothrombin g20210a.
Factor V Leiden is most common in the Caucasian population of European decent at 3-8% being carriers, and less common in other populations. Those with two copies (homozygous) is even more rare occurring in only approximate 1 in 5,000 people. [8]
Prothrombin g20210a is less common impacting approximately 1-3% of the general population. [8]
Persons with these genetic variants need to be more virulent about further stacking the hypercoagulation deck with additional clotting risk factors — i.e. estrogens/birth control pills, obesity, smoking, inflammation, certain vaccinations, etc.
If you have your 23andme genetic data, you can easily check for these yourself in your account using the links below.
Factor V Leiden gene F5 (risk allele T):
Because the genes present in this example are C / T, and T is the risk allele, this person would be heterozygous (one copy or a carrier) for F5 —Factor V Leiden. Carriers are said to have a 4 fold increase in blood clot risks vs. 11 fold increase for those who are homozygous ( T / T, or have two copies of the gene).
Prothrombin g20210a gene F2 (risk allele A):
Because the genes present in this example are G / G, and A is the risk allele, this person would not be a carrier, as they have two typical normal genes. Someone with A / G genes would be heterozygous, and someone with A / A genes would be homozygous.
NATURAL BLOOD SUPPORT
If you find yourself with a genetic predisposition for hypercoagulation, symptoms or conditional risk factors, it may be a good idea to check in with your doctor about how you can support your blood coagulation cascade and prevent blood clotting tendencies before it becomes a problem. Addressing toxicity and gut infections that could be congesting your gut-liver axis is key here.
Beyond prevention, two of my favorite natural supports are enzymes that break down fibrin in the blood, supporting the reduction of hypercoagulative states. Always check with your doctor before using substances that can thin the blood. Even natural blood thinners are contra-indicated in a variety of situations like pregnancy, breastfeeding, certain allergies, those taking specific medications and persons with bleeding disorders.
- Lumbrokinase:Lumbrokinase is an earthworm extract that has a long history of use in Chinese medicine for cardiovascular health. It’s known for its potent fibrin dissolving properties when taken on an empty stomach and can lower blood viscosity.
- Nattokinase:Nattokinase is an enzyme derived from fermented soybean (called natto) that supports the breakdown of soluble fibrin when taken on an empty stomach.
Additional support for hypercoagulative states:
- Dan Shen: Dan Shen is a herb used in traditional Chinese medicine to support vascular health and blood circulation. [12]
- Nitric Oxide Support: Nitric Oxide is a molecule that has anti-coagulant properties, opposes plaque formation, supports healthy blood pressure, and can reduce cholesterol levels. Levels of nitric oxide tend to decline after age 30, and are typically 50% less by age 45. Maintaining healthy levels of nitric oxide reduce the risks of cardiovascular disease. [13]
In short, addressing hypercoagulation can speed up healing, improve symptoms and sensitivity to treatment (thus outcome), and support an overall recovery from chronic illness.
I hope this helps you better understand your own body and what you can do to support it.